- 摘要
- 临床特征和诊断 Clinical characteristics and diagnosis
- 临床表现和检查 Clinical manifestations and workup
- 基因检测 Genetic testing
- 治疗 Treatment
- 管理和随访 Management and follow-up
- 总结和观点 Conclusion and perspectives
- 披露 Disclosure
- 致谢 Acknowledgments
- 补充材料 Supplementary Material
- 参考文献 References
本文链接:https://www.yuque.com/gs123/share/kdigo2016_gitelman_syndrome/
原文标题:Gitelman syndrome: consensus and guidance from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference
原文链接:https://www.kidney-international.org/article/S0085-2538(16)30602-0/fulltext30602-0/fulltext)
Anne Blanchard1,2,3,4, Detlef Bockenhauer5,6, Davide Bolignano7, Lorenzo A. Calo` 8, Etienne Cosyns9, Olivier Devuyst10, David H. Ellison11, Fiona E. Karet Frankl12,13, Nine V.A.M. Knoers14, Martin Konrad15, Shih-Hua Lin16,17 and Rosa Vargas-Poussou2,18
| 1 | 法国索邦巴黎大学联盟,笛卡尔大学医学院 |
|---|---|
| 2 | 法国乔治·蓬皮杜欧洲医院,巴黎援助公共医院,临床调查中心 |
| 3 | 法国巴黎国家德拉圣玛丽研究所,1418诊所调查中心 |
| 4 | UMR 970,法国国家健康与医学研究院 |
| 5 | 英国伦敦大学学院肾病学中心 |
| 6 | 英国伦敦国家健康服务信托基金大奥蒙德街儿童医院 |
| 7 | 意大利卡拉布利亚大区雷焦市国家研究委员会临床生理学研究院 |
| 8 | 意大利帕多瓦大学医学院肾病学系 |
| 9 | 比利时旺兹自治市 |
| 10 | 瑞士苏黎世大学生理学系 |
| 11 | 美国俄勒冈州,退伍军人事务部波特兰医疗保健系统,俄勒冈健康与科学大学肾病与高血压系 |
| 12 | 英国剑桥大学附属医院国家健康服务信托基金,剑桥大学医学遗传学系 |
| 13 | 英国剑桥大学附属医院国家健康服务信托基金会,剑桥大学肾脏医学专业 |
| 14 | 荷兰乌得勒支大学医学院分子医学中心遗传学系 |
| 15 | 德国明斯特大学儿童医院普通儿科 |
| 16 | 台湾台北国防医学院三军总医院医学系肾脏内科 |
| 71 | 台湾台北国防医学院医学科学研究所 |
| 18 | 法国巴黎儿童和成人遗传性肾病资料中心 |
通讯作者:
Olivier Devuyst, 瑞士苏黎世大学生理学系, Winterthurerstrasse 190, CH-8057, Zurich, Switzerland.
E-mail: olivier.devuyst@uzh.ch
或 Nine V.A.M. Knoers, 荷兰乌得勒支大学医学院分子医学中心遗传学系PO Box 85090, 3508 AB, Utrecht, the Netherlands. E-mail: v.v.a.knoers@umcutrecht.nl
上述作者均为本报告做出了同等贡献,按字母顺序排列。
国际肾脏杂志 (2017) 91, 24–33; http://dx.doi.org/10.1016/j.kint.2016.09.046
Copyright © 2016, International Society of Nephrology. Published by Elsevier Inc. This is an open access article under the CC BY-NC-SA license (http://creativecommons.org/licenses/by-nc-sa/4.0/).

摘要
Gitelman综合征(GS)是一种罕见的失盐性肾小管病变,其特征为低钾代谢性碱中毒伴低镁血症和低钙尿症。该疾病是隐性遗传,由编码噻嗪类敏感的钠氯协同转运蛋白(NCC)的SLC12A3基因中的失活突变引起。GS通常在青春期或成年期发现,可能是偶然或由轻度或非特异性症状而检查发现。该疾病的特征在于高表型多变性,以及生活质量的显著降低,并且可能伴有严重的临床表现。GS的疾病管理方法,通常是自由盐摄入以及口服镁和钾补充剂。罕见疾病的一个普遍问题是缺乏高质量证据为诊断,预后和管理提供信息。在此,我们汇报当前认识水平下GS的诊断评估,随访,管理和治疗方案; 找出认识缺漏;并提出研究议程,以确诊与GS有关的若干问题。本专家共识声明旨在建立初步框架,以实现临床审计(clinical auditing),从而提高医疗质量控制。
Gitelman syndrome (GS) is a rare, salt-losing tubulopathy characterized by hypokalemic metabolic alkalosis with hypomagnesemia and hypocalciuria. The disease is recessively inherited, caused by inactivating mutations in the SLC12A3 gene that encodes the thiazide-sensitive sodium-chloride cotransporter (NCC). GS is usually detected during adolescence or adulthood, either fortuitously or in association with mild or nonspecific symptoms or both. The disease is characterized by high phenotypic variability and a significant reduction in the quality of life, and it may be associated with severe manifestations. GS is usually managed by a liberal salt intake together with oral magnesium and potassium supplements. A general problem in rare diseases is the lack of high quality evidence to inform diagnosis, prognosis, and management. We report here on the current state of knowledge related to the diagnostic evaluation, follow-up, management, and treatment of GS; identify knowledge gaps; and propose a research agenda to substantiate a number of issues related to GS. This expert consensus statement aims to establish an initial framework to enable clinical auditing and thus improve quality control of care.
关键词:
低血钾代谢性碱中毒; 低镁血症; 失盐性肾小管病变; SLC12A3; 噻嗪类敏感的钠氯协同转运蛋白
hypokalemic metabolic alkalosis; hypomagnesemia; salt-losing tubulopathy; SLC12A3; thiazide-sensitive sodium-chloride cotransporter
Gitelman综合征(GS),也称为家族性低钾低镁血症,是一种失盐性肾小管病变,其特征为低血钾代谢性碱中毒伴低镁血症和低钙尿症1, 2 患病率约为每40,000人}1至10人,在亚洲可能更高,3 GS可能是最常见的遗传性肾小管病变。4 该病由SLC12A3基因中编码噻嗪类敏感的钠氯协同转运蛋白(NCC)的双等位基因的失活突变,在远曲小管的细胞顶膜中表达而引起。5 迄今为止,已有>350种分散在SLC12A3基因不同点位的突变在GS病人种发现。6, 7 大多数患者的SLC12A3突变是复合杂合突变,但是仍有较多GS患者仅携带单个SLC12A3突变。
Gitelman syndrome (GS), also referred to as familial hypokalemia-hypomagnesemia, is a salt-losing tubulopathy characterized by hypokalemic metabolic alkalosis with hypomagnesemia and hypocalciuria. With a prevalence at ∼1 to 10 per 40,000, and potentially higher in Asia, GS is arguably the most frequent inherited tubulopathy. The disease is caused by biallelic inactivating mutations in the SLC12A3 gene encoding the thiazide-sensitive sodium-chloride cotransporter (NCC) expressed in the apical membrane of cells lining the distal convoluted tubule. To date, >350 mutations scattered throughout SLC12A3 have been identified in GS patients. The majority of patients are compound heterozygous for SLC12A3 mutations, but a significant number of GS patients are found to carry only a single SLC12A3 mutation.
低钙尿症和低镁血症的存在是GS临床诊断的高度预兆,尽管低钙尿症的病因非常多样,并且可能没有低镁血症的情况。1, 8, 9 对于某些病例通过临床和生物学检查特征来区分其他失盐性肾病存在困难。一种包括低镁血症和低钙尿的GS类似表型,也与编码氯通道ClC-Kb的CLCNKB基因突变有关,ClC-Kb是经典型Bartter综合征(cBS或称Bartter综合征III型)的致病原因。ClC-Kb在远曲小管中的定位解释了与GS表型重叠的原因。10, 11 基因检测已越来越多地用于GS诊断,但仍然昂贵。
The presence of both hypocalciuria and hypomagnesemia is highly predictive for the clinical diagnosis of GS, although hypocalciuria is highly variable and hypomagnesemia may be absent. The use of clinical and biological features to differentiate from other salt-losing nephropathies is difficult in some cases. A GS-like phenotype, including hypomagnesemia and hypocalciuria, has also been associated with mutations in the CLCNKB gene encoding the chloride channel ClC-Kb, the cause of classic Bartter syndrome ([cBS] or Bartter syndrome type III). The localization of ClC-Kb in the distal convoluted tubule explains the phenotypic overlap with GS. Genetic testing is increasingly available for GS, but it remains expensive.
GS一直被认为是良性肾小管病变,通常在青春期或成年期发现。的确,该病可以没有任何症状,或仅有相对轻微或非特异性症状,例如:肌肉无力,疲劳,嗜盐,口渴,夜尿或痉挛。然而,这一观点受到强调表型多变性和该病潜在严重性的报道的挑战。12 Cruz等13 表明,GS与生活质量显著下降相关,相关性类似于充血性心力衰竭或糖尿病。严重的临床表现,例如早发(6岁前),生长迟缓,软骨钙质沉着,手足抽搐,横纹肌溶解,癫痫和室性心律失常。13, 14, 15 值得注意的是,在许多严重并发症的报告中,GS的诊断是基于临床而非基因检测,因此可能与包括经典性Batter综合征(cBS)在内的相关疾病产生混淆。然而,在基因证实的GS患者中也有表型多变性的记录,包括具有相同SLC12A3突变的患者。16 基因型、性别、修饰基因、代偿机制、环境因素或饮食习惯的不同都有可能影响这种多变性。17
GS has long been considered a benign tubulopathy, usually detected during adolescence or adulthood. Indeed, the condition may be asymptomatic or associated with relatively mild or nonspecific symptoms or both such as muscular weakness, fatigue, salt craving, thirst, nocturia, or cramps. However, this view has been challenged by reports emphasizing the phenotypic variability and potential severity of the disease. Cruz et al. showed that GS is associated with a significant reduction in the quality of life—similar to that associated with congestive heart failure or diabetes. Severe manifestations, such as early onset (before age 6 years), growth retardation, chondrocalcinosis, tetany, rhabdomyolysis, seizures, and ventricular arrhythmia have been described. Of note, in many reports of severe complications, the diagnosis of GS was established on clinical rather than genetic grounds, potentially creating confusion with related disorders including cBS. Yet, phenotypic variability has also been documented in genetically confirmed GS patients, including in patients with identical SLC12A3 mutations. A combination of genotype, sex, modifier genes, compensatory mechanisms, as well as environmental factors or dietary habits might be involved in such variability.
GS一般通过自由盐(NaCl)摄入以及口服镁和钾补充剂来管理。有时亦使用保钾利尿剂,肾素血管紧张素系统阻滞剂,例如:血管紧张素转换酶抑制剂和血管紧张素受体阻滞剂,以及非甾体抗炎药等。然而,在功效、耐受性和安全性方面,支持对GS患者使用这类治疗方案(单独或联合用药)的证据有限。缺乏GS患者长期结局的信息。特别需要考虑的是长期影响,如软骨钙质沉着症,慢性肾病,继发性高血压和心律失常,以及怀孕期间的管理。
GS is usually managed by a liberal salt (NaCl) intake, together with oral magnesium and potassium supplements. Potassium-sparing diuretics, renin angiotensin system blockers including angiotensin-converting-enzyme inhibitors and angiotensin receptor blockers, and nonsteroidal anti-inflammatory drugs are sometimes used. However, evidence supporting the efficacy, tolerability, and safety of these treatment options (either as standalone therapy or in combinations) in GS patients is limited. Information about long-term outcomes in GS is lacking. In particular, long-term consequences such as chondrocalcinosis, chronic kidney disease, secondary hypertension, and cardiac arrhythmias, and management during pregnancy need to be considered.
尽管自1996年以来,由于基因学解释,对GS的理解愈加深刻,但仍然存在许多谜团。以下问题需要进一步研究来证实:诊断标准和方法;临床检查和随访;表型异质性;生化异常和临床表现的本质和严重程度;以及治疗和疾病的长期影响。因此,改善全球肾病结局组织(KDIGO)主办了一次争议研讨会,以评估与当前GS相关的认识情况,找出认识漏缺,并提出研究议程。本报告总结了来自全球的多学科专家小组在本次会议上制定的临床实践和未来研究指南。
Despite the insights gained since its genetic elucidation in 1996, much mystery still surrounds GS. Further efforts are needed to substantiate issues including the following: diagnostic criteria and methods; clinical workup and follow-up; phenotypic heterogeneity; nature and severity of the biochemical abnormalities and clinical manifestations; and treatment and long-term consequences of the disease. Therefore, Kidney Disease: Improving Global Outcome (KDIGO) hosted a controversies conference to assess the current state of knowledge related to GS, identify knowledge gaps, and propose a research agenda. This report summarizes the guidance for clinical practice and future research developed at this conference by a global multidisciplinary panel of experts.
临床特征和诊断 Clinical characteristics and diagnosis
GS主要出现在青少年和成人中,但也可以在儿童中遇到,最早可发生在新生阶段。15, 18 关键的临床主诉和表现可作为GS诊断提示的 (表1) 包括如下情况:嗜盐(即,在童年时喜欢咸食或腌制的食物);肌肉无力,疲乏,运动能力或耐力低下;晕厥,痉挛,手足抽搐,感觉异样,手足痉挛;生长迟缓,青春期延迟,身材矮小;口渴或异常饮水行为;腹痛发作。成人可能会报告头晕、眩晕、多尿、夜尿、心悸、关节疼痛、视力下降等问题。
GS presents mainly in adolescents and adults but can also be encountered in children, as early as in the neonatal period. The key clinical complaints and manifestations suggesting a diagnosis of GS (Table 1) include the following: salt craving (i.e., preference for salty food or a salted treat during childhood); muscle weakness, fatigue, limited sport performance or endurance; episodes of fainting, cramps, tetany, paresthesia, carpopedal spasms; growth retardation, pubertal delay, short stature; thirst or abnormal drinking behavior; episodes of abdominal pain. Dizziness, vertigo, polyuria, nocturia, palpitations, joint pain, and visual problems may be reported in adults.
表1 | Gitelman综合征患者的临床表现 Clinical manifestations encountered in Gitelman syndrome patients
| 最常见的 (>50%) Most common (>50% of patients) |
显著的 (20%~50%) Prominent (20% ~ 50% of patients) |
偶发的 (< 20%) Occasional (<20%) |
罕见的 (个别报道) Rare (case reports) |
|---|---|---|---|
1. 嗜盐 1. 抽筋,肌肉无力 1. 乏力 1. 头晕 1. 夜尿 1. 口渴,烦渴 1. 感觉异样,麻木 1. 心悸 1. 低血压 |
1. 昏厥 1. 多尿 1. 关节痛 1. 软骨钙质沉着 1. QT间期延长 1. 发热 |
1. 早发(6岁前) 1. 发育停滞 1. 生长迟缓 1. 青春期延迟 1. 眩晕,共济失调 1. 手足痉挛,抽搐 1. 呕吐 1. 便秘 1. 遗尿 1. 麻痹 |
1. 癫痫发作 1. 室性心动过速 1. 横纹肌溶解症 1. 视力模糊 1. 假性脑瘤 1. 巩膜脉络膜钙化 |
1. Salt craving 1. Cramps, muscle weakness 1. Fatigue 1. Dizziness 1. Nocturia 1. Thirst, polydipsia 1. Paresthesia, numbness 1. Palpitations 1. Low blood pressure |
1. Fainting 1. Polyuria 1. Arthralgia 1. Chondrocalcinosis 1. Prolonged QT interval 1. Febrile episodes |
1. Early onset (before age 6) 1. Failure to thrive 1. Growth retardation 1. Pubertal delay 1. Vertigo, ataxia 1. Carpopedal spasm, tetany 1. Vomiting 1. Constipation 1. Enuresis 1. Paralysis |
1. Seizure 1. Ventricular tachycardia 1. Rhabdomyolysis 1. Blurred vision 1. Pseudotumor cerebri 1. Sclerochoroidal calcifications |
经许可改编自Devuyst等.83
Adapted, with permission, from Devuyst et al.
可作疑似GS诊断(表 2)的建议生化指标如下:
The proposed biochemical criteria for suspecting a diagnosis of GS (Table 2) include the following:
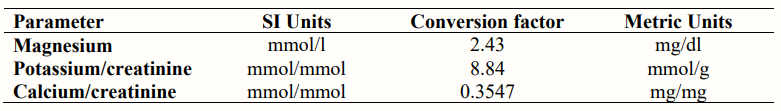
1. 没有使用降血钾药物的情况下,有记载的长期慢性低钾血症(<3.5 mmol / l)伴有不当的肾性失钾(随机尿,钾 - 肌酐比> 2.0 mmol / mmol [> 18 mmol / g]); 1. 代谢性碱中毒; 1. 低镁血症(<0.7 mmol / l [<1.70 mg / dl],[补充表S1]); [**补充表 1]**); 1. 不当的肾性失镁(镁排泄分数 > 4%); 1. 19, 20 低尿钙症(成人随机尿,钙 - 肌酐比<0.2 mmol / mmol [<0.07 mg / mg] [**补充表1**]; 1. 儿童钙 - 肌酐比值的正常范围与成人不同,详见 [补充表 2]);; 1. 高血浆肾素活性或水平; 1. 氯排泄分数 > 0.5%; 1. 正常或低血压; 1. 正常肾脏超声检查,无肾钙质沉着或肾脏异常; 1. 如病人服用钾或镁补充剂的一种或两种同时服用后的血浆电解质水平正常或接近正常值,则这些补充剂应停止至少48小时,以便发现可能的异常情况。血浆和尿液样本应同时采集。 1. 没有证据表明必须采集24小时尿液;随机尿液样本通常足以确定诊断。 |
|---|
- documented chronic hypokalemia (<3.5 mmol/l) concomitant with inappropriate renal potassium wasting (spot urine, potassium-creatinine ratio >2.0 mmol/mmol [>18 mmol/g]), in absence of potassium-lowering drugs;
- metabolic alkalosis;
- hypomagnesemia (<0.7 mmol/l [<1.70 mg/dl], [Supplementary Table S1]);
- inappropriate renal magnesium wasting (fractional excretion of magnesium >4%);
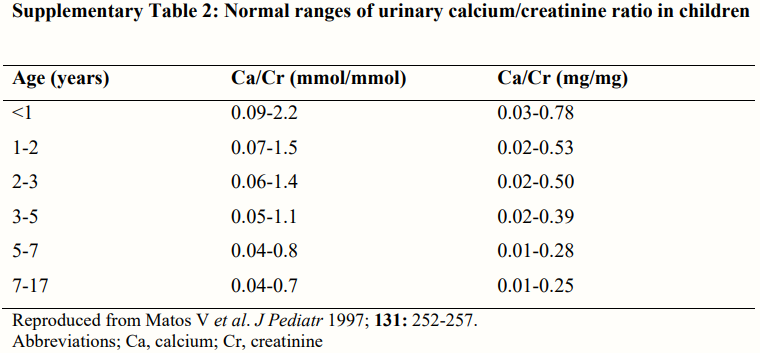
- hypocalciuria (spot urine, calcium-creatinine ratio <0.2 mmol/mmol [<0.07 mg/mg] in adults, [Supplementary Table S1];
- normal ranges of calcium-creatinine ratio are different in children, [Supplementary Table S2]);
- high renin (activity or plasma levels);
- fractional excretion of chloride >0.5%;
- normal or low blood pressure;
- normal renal ultrasound with absence of nephrocalcinosis or renal abnormalities.
- If plasma electrolyte levels are normal or close to normal in a patient taking potassium or magnesium supplements or both, these supplements should be stopped for at least 48 hours in order to potentially unmask the abnormalities. Plasma and urine samples should be obtained concomitantly.
- No evidence supports the need for 24-hour urine collection; spot urine samples are usually sufficient to establish the diagnosis.
表2 | Gitelman综合征的诊断标准 Diagnostic criteria for Gitelman syndrome
疑似GS的诊断标准 Criteria for suspecting a diagnosis of GS
1. 慢性低钾血症(<3.5 mmol / l),不当肾性失钾(随机 钾 - 肌酐比> 2.0 mmol / mmol [> 18 mmol / g]);
1. 代谢性碱中毒;
1. 低镁血症(<0.7 mmol / l [<1.70 mg / dl])伴有当的肾性失镁(镁排泄分数> 4%)
1. 成人中的低钙尿症(随机单次 钙 - 肌酐比率<0.2 mmol / mmol [<0.07 mg / mg])。**a**
1. 高血浆肾素活性或水平;
1. 氯排泄分数> 0.5%b
1. 低血压或正常血压;
1. 肾脏超声检查正常。
1. Chronic hypokalemia (<3.5 mmol/l) with inappropriate renal potassium wasting (spot potassium-creatinine ratio >2.0 mmol/mmol [>18 mmol/g])
1. Metabolic alkalosis
1. Hypomagnesemia (<0.7 mmol/l [<1.70 mg/dl]) with inappropriate renal magnesium wasting (fractional excretion of magnesium >4%)
1. Hypocalciuria (spot calcium-creatinine ratio <0.2 mmol/mmol [<0.07 mg/mg]) in adults.
1. High plasma renin activity or levels
1. Fractional excretion of chloride > 0.5%
1. Low or normal-low blood pressure
1. Normal renal ultrasound
不支持GS诊断的特征 Features against a diagnosis of GS
1. 使用噻嗪类利尿剂或泻药;
1. 有常染色体显性遗传的肾脏疾病家族史;
1. 无低钾血症(除非有肾功能衰竭的情况);
1. 未使用替代疗法的情况下,非持续性的低钾血症;
1. 无代谢性碱中毒(除非合并碳酸氢盐丢失或酸增加);
1. 低肾素;
1. 尿液:低尿钾排泄(随机单次 钾 - 肌酐比<2.0 mmol / mmol [<18 mmol / g]);
1. 高钙尿症;
1. 高血压,c细胞外液量增加的临床表现;
1. 肾脏超声:肾钙质沉着症,肾结石,单侧肾,囊性肾;
1. 产前羊水过多、肾脏强回声病史;
1. 3岁前发病。c
1. Use of thiazide diuretics or laxatives
1. Family history of kidney disease transmitted in an autosomal dominant mode
1. Absence of hypokalemia (unless renal failure);
1. inconsistent hypokalemia in absence of substitutive therapy
1. Absence of metabolic alkalosis (unless coexisting bicarbonate loss or acid gain)
1. Low renin values
1. Urine: low urinary potassium excretion (spot potassium-creatinine ratio <2.0 mmol/mmol [<18 mmol/g]);
1. hypercalciuria
1. Hypertension,c manifestations of increased extracellular fluid volume
1. Renal ultrasound: nephrocalcinosis, nephrolithiasis, unilateral kidneys, cystic kidneys
1. Prenatal history of polyhydramnios, hyperechogenic kidneys
1. Presentation before age 3 years
GS确诊标准 Criteria for establishing a diagnosis of GS:
测定SLC12A3中的双等位基因失活突变。
Identification of biallelic inactivating mutations in SLC12A3 |
| —- |
GS,Gitelman综合征 上述所列是根据已发表的证据和集体临床经验,支持或反对GS诊断的典型特征。 个体患者的特征可能存在差异,最终诊断需依赖于基因检测。因此,报告了3岁以前发病的情况,以及高血压(中年和老年GS患者中)和肾囊肿。84 a 由于儿童肌酐排泄较低,儿童的正常钙尿范围不同 (见补充表 2); b 氯排泄分数值是基于专家意见得出( 仅就尿氯的高多变性的问题),需根据已发表的临床观察验证; c 3岁前出现高血压和发病的,亦有GS可能性(见文本)。
GS, Gitelman syndrome. Listed are typical features arguing for or against a diagnosis of GS based on published evidence and collective clinical experience. Features in an individual patient may vary and ultimately the diagnosis rests on genetic testing. Thus, age of onset before 3 years of age has been reported, as has hypertension (in middle-aged and elderly patients with GS) and renal cysts. a Normal calciuria ranges are different in children due to lower creatinine excretion (see Supplementary Table S2). b The value of fractional excretion of chloride is based on expert opinion (high variability of urinary chloride alone) and requires verification from published clinical observations. c Hypertension and presentation before age 3 years do not exclude GS (see text).
不支持GS诊断的证据 (表 2) 包括以下方面:
- 肾脏畸形家族史或患有任何显性遗传的肾脏疾病;存在肾脏畸形(如单侧肾,多囊肾等);
- 羊水过多或高回声胎儿肾脏的病史;
- 3岁前发病;
- 长期使用利尿剂或泻药;
- 缺乏替代治疗时缺乏低钾血症或不一致的低钾血症;
- 无低钾血症,或在未使用替代疗法的情况下,非持续性的低钾血症;
- 长期高血压史;
- 细胞外液量增加的临床表现。
值得注意的是,成人动脉高血压的症状并不排除GS的可能性。21,22
Arguments against the diagnosis of GS (Table 2) include the following:
- a family history of renal malformations or any kidney disease dominantly transmitted;
- the presence of a renal malformation (e.g., unilateral kidneys, polycystic kidneys, etc.);
- a history of polyhydramnios or hyperechogenic fetal kidneys;
- presentation before age 3 years;
- chronic use of diuretics or laxatives;
- lack of hypokalemia or inconsistent hypokalemia in absence of substitutive therapy;
- long history of hypertension;
- manifestations of increased extracellular fluid volume.
Of note, the presence of arterial hypertension does not exclude the diagnosis of GS in adults.
临床疑似GS诊断的确认需依赖基因检测,应该向所有受试对象提供。测定双等位基因失活的SLC12A3突变可证明GS的诊断。鉴于基因检测的快速进展,氢氯噻嗪检测由于存在相应风险,不再推荐作为GS中的诊断工具:当它用于诊断时(即,区分Bartter综合征),有亨利袢缺陷的受试者存在急性容量不足的风险。8其他限制包括在儿童或服用影响肾小管转运过程的药物的患者中进行测试。氢氯噻嗪通常也可诱发急性间质性肾炎和过敏反应。除非出现特殊临床表现(例如,严重蛋白尿),否则对于GS的诊断没有必要使用肾活检。
Confirmation of clinically suspected GS rests on genetic testing, which should be offered to all subjects. The diagnosis of GS is proven by identification of biallelic inactivating SLC12A3 mutations. In view of the rapid progress of genetic testing, hydrochlorothiazide testing is no longer recommended as a diagnostic tool in GS because of the related risks: when it is used diagnostically (i.e., to differentiate from Bartter syndrome), there is a risk of acute volume depletion in subjects with loop of Henle defect. Other limitations include testing in children or in patients taking medications affecting tubular transport processes. Hydrochlorothiazide in general may also induce acute interstitial nephritis and hypersensitivity reactions. Unless specific manifestations (e.g., significant proteinuria) are encountered, a renal biopsy is not necessary for the diagnosis of GS.
GS的鉴别诊断包括经典型Batter综合征(cBS)。如症状出现在幼年(<3岁),存在生长发育迟滞、多尿且血镁正常,则后者可能性更大。然而,cBS和GS可能在临床上难以区分。**10, 11, 23**编码转录因子HNF1-β的HNF1B基因的突变导致的电解质异常(特别是低镁血症)与GS相似。HNF1B相关疾病的症状包括:成年发病、青年糖尿病、早年慢性肾病、显性遗传病家族史、肝酶异常、肾或泌尿生殖系统畸形或肾囊肿等。HNF1B突变可以在杂合状态下发生,无论是遗传的还是新生(de novo)变异的。HNF1B突变包括点位突变,和整个基因缺失。**24** 大约50%的患者由于肾性失镁而引起低镁血症,通常伴有低钙尿症,说明与远曲小管有关。**25** 编码内向整流钾离子通道Kir4.1的KCNJ10基于突变可导致以癫痫、共济失调、感应神经性耳聋和肾小管病变(或EAST综合征)为特征的常染色体隐性遗传病。EAST综合征的肾外特征可使其于GS区别开。**26**
The differential diagnosis of GS includes cBS. The latter is more likely when the presentation occurs at young age (<3 years), with failure to thrive, polyuria, and normal plasma magnesium levels. However, cBS and GS may be clinically indistinguishable. Mutations in the HNF1B gene encoding the transcription factor HNF1-β can mimic the electrolyte abnormalities (particularly hypomagnesemia) encountered in GS. The presence of maturity onset diabetes of the young, early chronic kidney disease, family history compatible with a dominant mode of inheritance, abnormal liver enzymes, renal or urogenital malformations or kidney cysts should point to HNF1B-related disorders. HNF1B mutations can occur in the heterozygous state, either inherited or de novo, and comprise point mutations as well as whole gene deletions. Approximately 50% of patients develop hypomagnesemia due to renal magnesium wasting, often accompanied by hypocalciuria, indicating that the distal convoluted tubule is involved.25 Mutations in the KCNJ10 gene coding for the inwardly rectifying potassium channel KCNJ10/Kir4.1 cause an autosomal recessive disorder characterized by epilepsy, ataxia, sensorineural deafness, and tubulopathy (or EAST syndrome). The extrarenal features of EAST syndrome allow it to be distinguished from GS.
GS的鉴别诊断还包括利尿剂和/或泻药滥用,这在儿童中很少见,以及慢性呕吐。测量尿氯(例如,<25 mEq / l 因自行诱导的呕吐 surreptitious vomiting )和尿液利尿剂检查(例如,通过质谱分析)可以帮助排除这些患者的GS可能性。 **27**低钾代谢性碱中毒与高肾素继发性醛固酮增多症的关联,可以在其他影响肾脏或胃肠道的家族性疾病中发现,或者也可以后天获得。例如,患有囊性纤维化的患者易发生低钠、低氯性脱水伴代谢性碱中毒。**28** 使用顺铂的可能出现类似GS症状的罕见并发症。**29 **自身免疫性疾病也可能导致肾小管疾病,这可能是由于自身抗体攻击肾小管组织造成的。**30 **GS的典型特征与自身免疫有关的症状包括虹膜炎和关节炎**31**和干燥综合征(Sjögren syndrome)**32**。
The differential diagnosis of GS also includes diuretic and/or laxative abuse, which is unusual in children, and chronic vomiting. Measurement of urinary chloride (e.g., < 25 mEq/l for surreptitious vomiting) and a urine screen for diuretics (e.g., by mass spectrometry) can help exclude GS in these patients. The association of hypokalemic metabolic alkalosis with hyperreninemic secondary aldosteronism is also found in other familial disorders affecting the kidneys or the gastrointestinal tract, or it can be acquired. For example, patients with cystic fibrosis are prone to develop episodes of hyponatremic, hypochloremic dehydration with metabolic alkalosis. GS-like manifestations have been reported as a rare complication of the use of cisplatin. Autoimmune disorders may cause renal tubular disorders, potentially due to autoantibodies against tubular components. Typical features of GS have been associated with autoimmune disorders including iritis and arthritis and Sjögren syndrome.
由于GS的罕见性,可能不会被当作一个单独疾病来诊断。因为临床表现可能是非特异性的,经常是在做生化检查时偶然发现。癫痫、生长迟缓、青春期延迟和神经肌肉等间接相关疾病的检查中应重视血钾和血镁指标。
Because of its rarity, GS may not be suspected as a distinct entity. As the clinical manifestations may be nonspecific, the disease is often discovered fortuitously during biochemical workup. The value of checking plasma potassium and magnesium levels in the workup of indirectly related conditions such as epilepsy, growth retardation, pubertal delay, and neuromuscular disorders should be stressed.
临床表现和检查 Clinical manifestations and workup
GS的大多数临床问题与电解质紊乱有关,特别是慢性失盐,低钾血症或低镁血症,也可能同时具备这些症状。越来越多的患者被诊断出来,说明对疾病的认识水平在不断提高,这有利于发现罕见并发症(表1),使得正确恰当的检查显得尤为重要。
Most of the clinical problems in GS are linked to electrolyte disturbances, in particular chronic salt loss, hypokalemia, or hypomagnesemia, or a combination of these. Increasing awareness of the disease is reflected by an increased number of patients identified, favoring the report of rare complications (Table 1) that should warrant the appropriate workup.
由于GS起源于远曲肾小管,GS患者的盐和水的丢失没有像产前Batter或经典型Batter(cBS)那么明显,因为GS的尿浓缩能力基本上完好无损。GS患者通常无症状或出现肌肉无力,乏力,嗜盐,口渴,夜尿,便秘,抽搐,手足痉挛或由低镁血症引发的强直搐搦等症状。33,34 血压通常较低,特别是对于低血钾、血镁严重的患者。35 GS的并发症包括软骨钙质沉着36和巩膜脉络膜钙化。37这是因为镁离子可增加焦磷酸钙晶体的溶解度,是组织非特异性碱性磷酸酶的重要激活因子,将焦磷酸盐(PPi)水解成无机磷酸盐(Pi)。因此,低镁血症可能增加关节和巩膜中焦磷酸钙晶体的形成。38 此外,肾脏钙重吸收的增加也可能促使钙沉积,而GS患者的骨矿物质密度较高,这种情况与慢性噻嗪类药物治疗相似,与骨重建速度下降有关。39,40 GS患者可能还存在生长迟缓,青春期延迟和身材矮小,反映了生长激素/类胰岛素生长因子I轴的改变,或由于生化指标异常导致的多效性。41 据报道,有几例严重GS患者导致低钾性横纹肌溶解症42。
Because GS originates from the distal convoluted tubule, the salt and water losses in GS patients are less pronounced than in antenatal BS or cBS because urinary concentrating ability is largely intact. GS patients are often asymptomatic or present with symptoms such as muscle weakness, fatigue, salt craving, thirst, nocturia, constipation, cramps, carpopedal spasms, or tetanic episodes triggered by hypomagnesemia. Blood pressure is typically low, particularly for patients with severe hypokalemia and hypomagnesemia. Complications of GS include chondrocalcinosis36 and sclerochoroidal calcifications. This is because magnesium ions increase the solubility of calcium pyrophosphate crystals and are important activators for tissue-nonspecific alkaline phosphatase, which hydrolyzes pyrophosphates (PPi) into inorganic phosphate (Pi), hence hypomagnesemia may promote the formation of calcium pyrophosphate crystals in joints and sclera. In addition, increased renal calcium reabsorption may contribute to calcium deposition, and patients with GS have higher bone mineral density, similar to chronic thiazide treatment, associated with a decreased rate of bone remodeling. They may also present with growth retardation, pubertal delay, and short stature, reflecting an alteration in the growth hormone/insulin-like growth factor I axis or pleiotropic effects resulting from the biochemical disturbance. Hypokalemic rhabdomyolysis has been reported in several GS patients.
如果出现疑似软骨钙质沉着症的特定症状,应行超声或X光检查。当怀疑巩膜脉络膜钙化时,需要进行眼科检查。37
Ultrasound or X-ray examination should be performed in case of specific complaints that are suggestive of chondrocalcinosis. Ophthalmology examination is indicated when sclerochoroidal calcifications are suspected.
钾和镁的减少会延长心肌细胞动作电位时程(APD),导致约50%的GS患者QT间期延长,这可能增加室性心律失常的风险。43,44 已有GS患者长期室性心动过速的报道。14 鉴于已有GS患者心律失常、长QT、猝死的个别报道,应给患者做静息心电图(ECG)以评估心率和QT间期。如患者主诉心悸、眩晕,或经治疗生化指标改善后心电图持续异常,则应做进一步的心脏病学检查(如:动态心电图、运动心电图)。45
Potassium and magnesium depletion prolong the duration of the action potential in cardiomyocytes, resulting in prolonged QT interval in ∼50% of the patients, which could lead to an increased risk for ventricular arrhythmias. GS patients who presented with long runs of ventricular tachycardia have been reported. Given isolated reports on cardiac arrhythmias, long QT and sudden death in GS, an electrocardiogram (ECG) should be performed at rest to assess rhythm and QT duration. A further cardiology workup (e.g., Holter, stress ECG) is indicated where patients complain of palpitations or syncope, or if the ECG abnormalities persist despite attempted improvement of the biochemical abnormalities.
GS患者可能由于慢性低镁血症和低钾血症,继发糖耐量异常,或胰岛素抵抗,或两者皆有。46 尽管如此,也有报道,由于血管紧张素II信号传导减弱和氧化应激减少,胰岛素敏感性提高,对动脉粥样硬化的形成亦有防护作用。47,48
Patients with GS may present glucose intolerance or insulin resistance or both secondary to chronic hypomagnesemia and hypokalemia. Nevertheless, increased insulin sensitivity and protection from atherogenesis due to blunted angiotensin II signaling and reduced oxidative stress have also been reported.
报告表明,由于肾小球基底膜异常,GS可能会导致肾小球蛋白尿。22,49 GS可能有诱发慢性肾病的风险,原因可能是由于长期低血钾与肾小管间质性肾炎、肾小管空泡变性和囊性改变有关,或者是由于容量不足和肾素 - 血管紧张素 - 醛固酮增加而导致的肾损害和纤维化。21,50,51
Reports suggest that GS may be associated with glomerular proteinuria due to abnormalities of the glomerular basement membrane. Chronic kidney disease might develop in GS patients due to either chronic hypokalemia, which is associated with tubulointerstitial nephritis, tubule vacuolization, and cystic changes, or volume depletion and increased renin-angiotensin-aldosterone, which may contribute to renal damage and fibrosis.
许多GS患者,可能是由于低钾血症引起的肠轻瘫或钾镁补充剂不耐受,而出现腹痛。这些症状应进行相应的检查并处理。还有报道,GS患者出现肾脏磷代谢受损。52
Many patients with GS present with abdominal pain, which may be due to intestinal paresis because of hypokalemia or intolerability of potassium and magnesium supplementation. These complaints should be investigated appropriately and treated accordingly. Impaired renal phosphate handling has also been reported.
基因检测 Genetic testing
GS的诊断中至关重要是检测是否存在SLC12A3双等位基因的失活突变。GS基因测试的分析敏感性(即,当SLC12A3外显子或外显子-内含子边界中存在的2个突变时,阳性结果的比例)和特异性(即,当SLC12A3中不存在2个突变时,阴性结果的比例)分别为90%~100%和100%。因为有些患者的SLC12A3基因中没有2个突变(也就是说,有一个突变位于非编码区或在其他基因中,没有被包含在检测范围内),临床敏感性(存在明显症状时,阳性检测结果的比例)受所使用的基因检测方法的影响,在65%至80%。7,12,50,53,54,55 致病性SLC12A3突变包括大段的重排(缺失),其可通过多重连接探针扩增技术测定,7 还包括内含子突变,可使用淋巴细胞cDNA分析检查。50,56 随着基因检测变得更加普及和全面,应该提供给所有临床疑似GS患者(按最低检测要求)。并应在具备(临床)诊断级基因检测资质的实验室中进行。
The detection of biallelic inactivating SLC12A3 mutations is crucial for the diagnosis of GS. The analytical sensitivity (i.e., the proportion of positive tests if 2 mutations in the SLC12A3 exons or exon-intron boundaries are present) and specificity (i.e., proportion of negative tests if 2 mutations in SLC12A3 are not present) of genetic testing for GS is 90% to 100% and 100%, respectively. Because there are GS patients who do not have 2 mutations in SLC12A3 (i.e., a mutation in the noncoding regions or in another gene, which are not included in the test), the clinical sensitivity (proportion of positive tests if the disease is present) is 65% to 80%, depending on the genetic methods used. Pathogenic SLC12A3 mutations include larger rearrangements (deletions), which can be picked up by multiplex ligation-dependent probe amplification, and intronic mutations, which can be screened for by cDNA analysis of lymphocytes. As genetic testing becomes more accessible and comprehensive, it should be offered to all patients with a clinical suspicion of GS (minimal criteria). It should be performed in a laboratory accredited for diagnostic genetic testing.
推荐使用下一代基于测序的基因panel对与GS鉴别诊断相关的基因进行平行序列(在1次检测中)。下一代测序基因panel有多种可选;但应该至少包括SLC12A3、CLCNKB和HNF1B基因。如果通过下一代测序Panel测序仅发现一个了单个变异,则应该对另一个等位基因的缺失(多重连接依赖性探针扩增)测试进行补充。如果实验室条件只能做桑格(Sanger)测序,则应对SLC12A3,CLCNKB和HNF1B进行顺序测试。如有必要,还应对这些基因进行多重连接探针扩增技术检测作为补充手段。
The use of a next generation sequencing–based gene panel to parallel sequence (in 1 test) all genes that are relevant in the differential diagnosis of GS is recommended. Different next generation sequencing gene panels are available; it should at least include the SLC12A3, CLCNKB, and HNF1B genes. If only a single variant has been identified by next generation sequencing panel sequencing, the analysis should be complemented with a test for a deletion (multiplex ligation-dependent probe amplification) on the other allele. If Sanger sequencing is the only available technique in the diagnostic lab, sequential testing of SLC12A3, CLCNKB, and HNF1B should be performed, and if necessary complemented by multiplex ligation-dependent probe amplification testing for these genes.
必须牢记的是,即使在多重连接探针扩增分析后,仍有15%~20%的患者7,57 只发现了1个致病突变。7 对于这些病例,基因调节区的突变,如SLC12A3的内含子,或另其他基因的突变可能是潜藏的另一个分子缺陷。目前,这些突变仅在特定情况下进行检测(例如,严重病例、亚裔背景、遗传咨询目的等),但随着下一代测序技术在诊断实验室中的普及,这种情况可能随之改变。
It must be kept in mind that in 15% to 20% of patients, even after multiplex ligation-dependent probe amplification analysis, only 1 pathogenic mutation is discovered. In these cases, mutations in regulatory regions including introns of SLC12A3 or in another gene might be the underlying second molecular defect. At present, these mutations are only searched for in specific cases (e.g., severe cases, Asian background, genetic counseling purposes), but this may change with dissemination of next generation sequencing techniques in diagnostic labs.
GS患者,和患有GS的幼儿的父母都应接受遗传咨询。可建议父母、兄弟姐妹和配偶进行基因检测。当确定2个致病性SLC12A3突变时,产前诊断和胚胎植入前遗传学诊断(PGD)在技术上是可行的。根据我们的经验,由于大多数GS患者预后良好,因此这类检查尚未推广。对于非常严重的病例,可考虑使用这类预测性检测。
Genetic counseling should be offered to any patient with GS and to parents with a young child suffering from the disease. This counseling could discuss testing of parents, siblings and partner. Prenatal diagnosis and preimplantation genetic diagnosis are technically feasible when 2 pathogenic SLC12A3 mutations have been identified. In our experience, these tests have not been asked for because of the good prognosis in the majority of GS patients. In very severe cases, the possible use of these predictive tests could be potentially discussed.
在不久的将来,全外显子组测序和全基因组测序,然后再进行靶向分析,将成为许多疑似遗传疾病患者优先考虑的基因检测方式。在做这类遗传筛查检测之前,始终应该先(给患者)进行细致的遗传咨询,并得到明确的知情同意。58 值得注意的是,随着基于新的群体基因数据和功能研究的日益普及,变异的分类可能会有变化:原先的疾病相关的基因变异的致病性可能会受到质疑,反之亦然,先前未知的相关变异可能被证明为致病性变异。59 诊断实验室应考虑到不断进化的人群,并考虑体外(in vitro)研究以恰当地解释患者的检测结果。60
In the near future, whole exome sequencing and whole genome sequencing, followed by targeted analysis, will become the genetic tests of preference in many patients with a presumed genetic disorder. Careful genetic counseling and specific informed consent should always precede those genetic screening tests. It is important to note that with the increasing availability of new-population–based genetic data and functional studies, the classification of variants may change: the pathogenicity of previously disease-associated genetic variants could be questioned and, vice versa, variants of previously unknown significance could be confirmed as pathogenic. Diagnostic laboratories should take into account the evolving population and consider in vitro studies to interpret patient results appropriately.
治疗 Treatment
由于GS是由氯化钠协同转运蛋白的主要缺陷引起的,因此应大力提倡自由摄入NaCl。我们建议鼓励GS患者保持他们嗜盐的习惯。迄今为止,在自由盐摄入的基础上增加药物性NaCl补充剂的潜在益处,尚无试验证明。
Because GS is caused by a primary defect in a sodium-chloride cotransporter, ad libitum NaCl intake should be strongly advocated. We recommend to encourage patients to follow their propensity for salt consumption. As yet, the potential benefit of pharmacological NaCl supplements added to liberal salt intake has not been tested.
个体化的终身口服钾或镁补充剂,或合并使用,是GS患者的核心治疗方法。在存在低镁血症的情况下,补镁应首先考虑。因为补镁会提高钾的补充效果,并降低手足抽搐和其他并发症的风险。19,33
Individualized lifelong oral potassium or magnesium supplementation or both is the mainstay of treatment for patients with GS. In the presence of hypomagnesemia, magnesium supplementation should be considered first, because magnesium repletion will facilitate potassium repletion and reduce the risk of tetany and other complications.
补充钾、镁后,GS的很多症状可得到改善。但没有证据表明,血液(指标)水平的严重程度与症状轻重有相关性。较为合理的目标值是:钾3.0mmol/l,和镁0.6mmol/l(1.46mg/dl)。一些患者可能很难达到这样的目标值,并且大剂量的补充钾/镁可能产生严重的副作用,如:胃溃疡、呕吐、腹泻,从而使生化指标更加恶化。应根据个体情况,在血液指标的改善目标、和副作用之间的建立平衡。某些患者的实际目标值可以更低,但也可能随时间而变化。钾/镁补充剂的依从性可能会受到用药成本的影响 - 因为不同国家的医药费用报销政策不同。
Many symptoms are improved by potassium or magnesium supplementation or both, but there is no evidence correlating the severity of blood levels with the intensity of symptoms. A reasonable target for potassium may be 3.0 mmol/l and magnesium 0.6 mmol/l (1.46 mg/dl). Achieving these targets can be difficult in some patients and supplementation with large doses may result in serious side effects including gastric ulcers, vomiting, or diarrhea with worsening biochemistries. An individual balance between improvement in blood values and side effects should be established. Realistic target values may be lower for some patients and may also change with time. Adherence to the supplementation may be influenced by cost—because variable reimbursement policies exist in different countries.
钾补充剂应使用氯化物(KCl),因为氯化物是尿液中主要丢失的阴离子,而患者是碱中毒的。KCl的建议起始剂量是 ≥40mmol(儿童 1-2mmol/kg),全天分次补充。钾补充剂不应空腹服用,以尽量减少胃肠道刺激或伤害。根据患者的个人偏好不用,KCl补充剂可以用水剂、制成糖浆或缓释剂等形式给药。已知维持剂量可能较高,剂量应根据个体情况滴定测量(副作用 vs. 症状)。推荐患者食用富含钾的食物,但要注意其中一些高碳水和高卡路里食物(补充表3)。
Potassium supplements should be given as chloride (KCl) because chloride is the main anion lost in the urine and patients are alkalotic. A starting dose of ≥40 mmol KCl (1–2 mmol/kg in children), in divided doses throughout the day, is suggested. Potassium supplements should not be taken on an empty stomach to minimize gastrointestinal irritation or damage. KCl supplements can be administered in water, as syrup, or in a slow-release formulation according to each patient’s preference. The dose will be titrated individually (side effects vs. symptoms), knowing that the maintenance dose may be high. Potassium-rich foods should be recommended, with the caution that some of them contain high carbohydrates and calories (Supplementary Table S3).
当患者不能口服药物,或低钾非常严重时,导致心律失常、四肢麻痹、呼吸衰竭或横纹肌溶解时,应考虑静脉补钾。61 KCl应用生理盐水稀释,通常浓度为40 mmol/L。一般来说,通过外周静脉以不超过10 mmol/h的最大速率输液不应超过50mmol/L,因为更高浓度的钾刺激性很强,可导致静脉疼痛和硬化。对于中心静脉,最大浓度通常为80 mmol / l,最大速率为20 mmol / h(取决于低血钾、ECG心电监护情况)。超过10 mmol / h时,应在高依赖环境或病房(HDU)对患者进行监护。服用外源性钾补充剂的患者如出现急性肾功能衰竭时,可能会出现严重的高钾血症。62
Intravenous KCl may be necessary either when the patient cannot take oral drugs or when the potassium deficit is very severe, causing cardiac arrhythmias, quadriplegia, respiratory failure, or rhabdomyolysis. KCl should be diluted in saline, usually to a concentration of 40 mmol/l. In general, no more than 50 mmol/L should be given through a peripheral vein at a maximum rate of 10 mmol/h, because higher concentrations of potassium are very irritating, resulting in pain and sclerosis of the vein. For central venous lines, the maximum concentration is usually 80 mmol/l with a maximum rate of 20 mmol/h (depending on hypokalemia, ECG monitoring). Beyond 10 mmol/h, the patient should be monitored in a high-dependency environment or area. Severe hyperkalemia may develop when acute renal failure develops in a patient taking exogenous potassium supplementation.
口服镁补充剂是纠正镁缺乏的首选方式。低镁会加重低钾血症状并使其难以通过补钾治疗纠正。63 所有类型的镁盐都是有效的,但生物利用度差别很大(补充表S4),高剂量使用时会发生渗透性腹泻。64有机盐(如:天冬氨酸盐、枸橼酸盐、乳酸盐)比氧化镁和氢氧化镁具有更高的生物利用度。64 MgCl2还可以补偿尿液中的氯离子损失。镁元素推荐起始剂量是300毫克/天(12.24 mmol),(儿童5 mg/kg,即0.2mmol/kg),如果有条件,缓释片剂更佳。补充剂应分为2~4次服用,随餐服用为宜。根据血液指标和肠耐受性,通常有必要进行剂量滴定。发生持续性腹泻必须减少用药剂量,这样反而可能提高血镁水平,这可能是由于(腹泻减轻后)生物利用度提高,或肠道传输时间减少。65 补充表S5中提供了富含镁的食物清单。
Oral administration of magnesium supplements is the preferred way to correct magnesium deficiency, which aggravates hypokalemia and renders it refractory to treatment by potassium. All types of magnesium salts are effective, but their bioavailability is highly variable (Supplementary Table S4), resulting in osmotic diarrhea at high doses. Organic salts (e.g., aspartate, citrate, lactate) have a higher bioavailability than magnesium oxide and hydroxide.64 MgCl2 will also compensate the urinary loss of chloride. The recommended starting dose is 300 mg/day (12.24 mmol) of elemental magnesium (5 mg/kg in children, i.e., 0.2 mmol/kg), in slow-release tablets when possible. The supplementation should be divided into 2 to 4 doses, preferably with meals. Dosage titration based on blood levels and intestinal tolerance is usually necessary. Persistent diarrhea may mandate a drop in dosage, which paradoxically may improve serum levels thanks to increased bioavailability or decreased intestinal transit time or both. A list of magnesium-rich foods is provided in Supplementary Table S5.
如患者出现急性、严重的低镁血症并发症(例如:手足抽搐,心律失常)或口服补充剂消化道不耐受的情况,则应考虑静脉补镁。在急性手足抽搐的情况下,应静脉注射20%MgCl2(每剂0.1 mmol Mg / kg),并可每6小时重复一次。4
Intravenous infusion of magnesium should be reserved either for patients presenting with acute, severe complications of hypomagnesemia (e.g., tetany, cardiac arrhythmias), or in cases of digestive intolerance to oral supplements. In cases of acute tetany, 20% MgCl2 should be administered intravenously (0.1 mmol Mg/kg per dose) and can be repeated every 6 hours.
如果药物依从性足够,但依然剂量不足,或副作用严重的情况下,长期低钾症状难以改善。则建议使用保钾利尿剂、66,67肾素-血管紧张素系统阻滞剂68,非甾体类抗炎药(如:吲哚美辛(消炎痛)),或上述药物联合用药治疗。69,70,71 保钾利尿剂(阿米洛利、安体舒通、坎利酸钾和依普利酮等)可用于提高钾镁补充剂抗拒患者的血钾水平,并治疗由醛固酮水平升高66造成的失镁。安体舒通由于其抗雄性激素作用,可诱发诸如男性乳房发育、多毛症、勃起障碍、月经失调等并发症。在青少年和年轻人中(安全)使用难度更大。依普利酮是一种选择性醛固酮拮抗剂,对雄激素、黄体酮和糖皮质激素受体的亲和性显著低于安体舒通,因此没有抗雄激素副作用。72 这些药物可加重肾性失盐,因此应谨慎使用以避免低血压。应考虑同时补盐。
In cases of persistent, symptomatic hypokalemia when supplements are not sufficient despite adherence or when side effects are unacceptable or both, the use of potassium-sparing diuretics, renin angiotensin system blockers, or nonsteroidal anti-inflammatory drugs, such as indomethacin, or a combination of these have been proposed. The potassium-sparing diuretics amiloride, spironolactone, potassium canrenoate, and eplerenone can be useful, both to increase serum potassium levels in patients resistant to supplements and to treat magnesium depletion that is worsened by elevated aldosterone levels. The use of spironolactone is complicated by its antiandrogenic effects such as gynecomastia, hirsutism, erectile dysfunction, and menstrual irregularities, which are particularly difficult in adolescents and young adults. Eplerenone is a selective aldosterone antagonist, with significantly lower affinity for androgen, progesterone, and glucocorticoid receptors in comparison with spironolactone and has therefore no antiandrogenic side effects. These drugs compound the renal salt wasting and should thus be started cautiously to avoid hypotension. Concomitant salt supplementation should be considered.
在GS的治疗中,偶有报道使用肾素血管紧张素系统抑制剂(血管紧张素转换酶抑制剂和血管紧张素受体阻滞剂)68。这些药物也会加重肾脏失钠,并增加症状性低血容量的风险;如果出现严重的失盐并发症,应停止用药,如:呕吐、腹泻。前列腺素合成酶抑制剂如吲哚美辛(消炎痛)很少用于GS治疗,因为GS中的前列腺素E2水平通常是正常的。环氧化酶-2(COX-2)抑制剂罗非昔布(Rofecoxib)也被用于顽固性低钾血症的治疗71,但该药物由于其对心血管的长期影响应慎重使用。
The use of renin angiotensin system inhibitors (angiotensin-converting-enzyme inhibitors and angiotensin receptor blockers) has been occasionally reported in the treatment of GS. These drugs also aggravate renal sodium wasting and increase the risk of symptomatic hypovolemia; they should be stopped in case of acute, salt-losing complications, such as vomiting or diarrhea. Prostaglandin synthase inhibitors such as indomethacin are rarely used in GS, because urinary prostaglandin E2 levels in GS are usually normal. Refractory hypokalemia has also been treated with the specific COX-2 inhibitor rofecoxib, but the use of this drug is limited by its long-term cardiovascular effects.
最近,有一项为期6周的针对30名GS患者的开放性随机交叉研究。方法是,在固定的钾镁补充剂基础上,按每日一次用药的方式,对比了多种药物的效果和安全性,分别是:吲哚美辛(消炎痛)缓释剂 75毫克 ,依普利酮150毫克,或阿米洛利20毫克。73 每种药物都使血钾浓度增加约0.3 mmol / l。阿米洛利和依普利酮加重钠消耗,而吲哚美辛(消炎痛)与肾小球估算滤过率降低相关,并且三分之一的受试者出现胃肠不耐受。虽然已有报道证明吲哚美辛(消炎痛)对低钾血有效,但由于其短期和长期的胃肠道副作用和肾毒性,应谨慎使用吲哚美辛(消炎痛)和其他非甾体类抗炎药。
Recently, an open-label, randomized, crossover study was conducted to compare the efficacy and safety of 6-week treatment with once-daily doses of 75 mg slow-release indomethacin, 150 mg eplerenone, or 20 mg amiloride added to constant potassium and magnesium supplementation in 30 GS patients. Each drug increased plasma potassium concentration by about 0.3 mmol/l. Amiloride and eplerenone aggravated sodium depletion, whereas indomethacin was associated with decreased estimated glomerular filtration rate and caused gastrointestinal intolerance in one-third of subjects. Despite a documented effect on hypokalemia, indomethacin and other nonsteroidal anti-inflammatory drugs should be used with caution due to their short- and long-term gastrointestinal side effects and nephrotoxicity.
GS患者应避免或慎用一系列药物(表3)。包括减缓窦性心律或影响QT间期的药物(例如,负性变频药物),可能加重低镁血症的药物(例如,质子泵抑制剂、庆大霉素、抗病毒药物)和乙酰唑胺。
A series of drugs should be avoided or used with caution in patients with GS (Table 3). These include drugs slowing sinus rhythm or influencing the QT interval (e.g., negative chronotropic drugs), drugs potentially exacerbating hypomagnesemia (e.g., proton-pump inhibitors, gentamicin, antiviral drugs), and acetazolamide.
表3 |与低钾血症和低镁血症相关的药物
| 丢失点 Site of loss | 药物 Drugs | |
|---|---|---|
| 低钾血症 Hypokalemia | ||
| 从细胞外液转移到细胞内液 Shift from extracellular fluid to intracellular fluid compartment |
β2受体激动剂 β2-receptor agonists 胰岛素(高剂量)联合葡萄糖 Insulin (high dose) with glucose 黄嘌呤药物(茶碱,咖啡因)Xanthines (theophylline, caffeine) 维拉帕米(过量使用) Verapamil (in overdose) 碳酸氢钠 Sodium bicarbonate |
|
| 肾外 Extrarenal | 泻药 Laxatives | |
| 肾脏 Renal |
抗菌药物 Antimicrobials |
萘夫西林、氨苄西林、青霉素、氨基糖苷类、两性霉素B、膦甲酸钠 Nafcillin, ampicillin, penicillin, aminoglycosides, amphotericin B, foscarnet |
| 利尿剂 Diuretics |
乙酰唑胺、呋塞米和其他髓袢利尿剂、噻嗪类、甘露醇 Acetazolamide, Furosemide and other loop diuretics, Thiazides, Mannitol |
|
| 盐皮质激素 Mineralocorticoids |
氟氢可的松 Fludrocortisone | |
| 抗癫痫药 Antiepileptic |
托吡酯 Topiramate | |
| 低镁血症 Hypomagnesemia | ||
| 肾外 Extrarenal | 质子泵抑制剂 Proton pump inhibitor | |
| 肾脏 Renal |
抗菌药物 Antimicrobials |
药物性肾范可尼综合征:氨基糖苷类(庆大霉素、链霉素、妥布霉素)、喷他脒、两性霉素B、膦甲酸钠、抗逆转录病毒治疗 Drug-induced renal Fanconi syndrome: Aminoglycosides (gentamycin, streptomycin, tobramycin), pentamidine, amphotericin B, foscarnet, antiretroviral therapy |
| 利尿剂 Diuretics |
呋塞米、噻嗪类利尿剂 Furosemide, Thiazide | |
| 抗肿瘤药 Antitumoral |
顺铂、酪氨酸激酶抑制剂 Cisplatin, Tyrosine kinase inhibitors | |
| 免疫抑制剂 Immunosuppressants |
钙调磷酸酶抑制剂(环孢霉素、他克莫司) 麦考酚酯 抗EGF受体(西妥昔单抗、帕尼单抗) Calcineurin inhibitors (cyclosporine, tacrolimus) Mycophenolate Anti-EGF receptors (cetuximab, panitumumab) |
EGF,表皮生长因子。 另见 Sung等。85,86
EGF, epidermal growth factor. See also Sung et al
补镁是预防软骨钙质沉着症的基础。治疗急性软骨钙质沉着症,可口服非甾体类抗炎药和低剂量口服秋水仙碱,两者都是有效的全身性治疗方法74,75。由于肾损伤的风险,GS患者必须谨慎使用非甾体类抗炎药。然而,秋水仙碱用药可以增加口服镁补充剂的致泻作用。对于存在其他药物禁忌或不耐受的患者,可考虑使用关节内注射类固醇激素。对于患有严重软骨钙质沉着症的患者,已有报道建议可间歇性使用一般皮质类固醇以及甲氨蝶呤。76
The cornerstone of the prevention of chondrocalcinosis is magnesium supplementation. Both oral nonsteroidal anti-inflammatory drugs and low-dose oral colchicine are effective systemic treatments for acute chondrocalcinosis. Nonsteroidal anti-inflammatory drugs have to be used with caution in GS due to risk of kidney injury, whereas colchicine treatment can increase the laxative effect of oral magnesium supplementation. Intra-articular corticosteroids may be considered in patients in whom other drugs are contraindicated or not tolerated. Intermittent general corticosteroids, as well as methotrexate, have been proposed for patients with severe chondrocalcinosis.
管理和随访 Management and follow-up
GS患者的管理应该个性化,并随着时间和需求的变化而相应调整。至少每年在肾脏门诊进行一次随访,以监测潜在的并发症和病情进展。无论低钾血症的控制情况如何,症状都可能随着年龄的增长而加重。绝经后低血钾症状可能更容易控制。应教育患者悉知钾镁补充剂的副作用,特别是镁盐引起的腹痛和腹泻,以及氯化钾对胃的刺激。医生还应该注意可能影响钾镁补充剂药物依从性的其他因素,包括:社会经济困难、缺乏医保报销、青春期、(儿童、青少年到成人的)过渡期、工作环境等。从儿科到成人治疗之间的过渡阶段尤为重要。
The management of GS should be individualized, with appropriate change with time and demands. At least annual follow-up in a nephrology clinic to monitor potential complications and evolution is advocated. The symptoms may increase with aging, irrespective of the control of hypokalemia. The latter may be easier after menopause. Patients should be educated about side effects of the supplements, in particular abdominal pain and diarrhea induced by magnesium salts and gastric irritation from potassium chloride. Physicians also should be attentive to other factors that could hamper adherence to the supplements, including socioeconomic difficulties, lack of reimbursement, adolescence, transition period, work conditions, etc. The transition phase between pediatric and adult care is particularly important.
需要进行长期研究,以评估GS的自然病史,以及慢性低钾血症、低镁血症的个别风险,包括:代谢综合征、心律失常、慢性肾病、血压控制和软骨钙质沉着症的发展倾向等。迄今为止,没有证据表明GS会影响预期寿命。
Long-term studies are needed to assess the natural history of GS and the individual risks of chronic hypokalemia and hypomagnesemia in terms of metabolic syndrome, cardiac arrhythmias, chronic kidney disease, blood pressure control, and propensity to develop chondrocalcinosis. To date, there is no evidence that GS affects life expectancy.
妊娠期间低钾血症和低镁血症的病情会加重,需要肾内科和产科尽早建立联合管理机制,并相应调整补充剂用药方案。77,78,79 迄今为止,报道的GS妊娠母亲和胎儿的结局良好,母亲或胎儿都未报道出现心律失常或其他严重心脏并发症的案例。77,78 需要重视的是,由于对胎儿存在严重风险,怀孕期间应停止使用血管紧张素受体阻滞剂和血管紧张素转换酶抑制剂。80,81 建议在分娩期间监护血浆电解质水平。分娩后,母亲有可能恢复到最基础的补充剂用量和随访要求。
The known aggravation of hypokalemia and hypomagnesemia during pregnancy requires the early institution of a joint management plan involving nephrology and specialized obstetrics, as well as appropriate adaptations in the supplementation. The outcome of mother and fetus of GS pregnancies described to date is favorable, with no cases of arrhythmia or other serious cardiac complication reported for either the mother or fetus. Importantly, angiotensin receptor blockers and angiotensin-converting-enzyme inhibitors should be stopped during pregnancy because of significant fetal risks. Monitoring of plasma electrolyte levels is advised during labor. After delivery, the treatment of the mother may return to baseline supplementation and follow-up.
GS患者接受麻醉时应谨慎。低钾血和低镁血症可以增强局部和全身麻醉剂的作用(例如,在全身麻醉期间和区域阻滞中使用肾上腺素时,出现神经肌肉阻滞)。目前尚无权威证据,对术前钾和镁的安全水平有明确建议。对于一般人群,英国国家健康和护理优化研究所(NICE)批准的指南中建议的目标值是,钾≥3.0mmol/L,镁0.5 mmol/L(1.22 mg / dl)。82
Caution should be taken when patients with GS undergo anesthesia. Hypokalemia and hypomagnesemia can potentiate the effects of local and general anesthetic agents (e.g., neuromuscular blockade during general anesthesia and adrenalin use in regional blockade). There is no definitive evidence to suggest exact preoperative levels of potassium and magnesium that are safe. In the general population, the UK National Institute for Health and Care Excellence (NICE)-approved guidelines suggest aiming for potassium levels of ≥3.0 mmol/l and magnesium 0.5 mmol/l (1.22 mg/dl).
GS儿童的电解质紊乱会造成青春期和生长迟缓。12 如果已进行足够的钾镁补充剂治疗,仍然出现显著的生长发育问题,则建议对青春期状态和生长激素水平进行正式评估。如果生化指标控制得当,生长激素治疗对明确的生长激素缺乏患者通常是有帮助的。
The electrolyte disturbances in children with GS are associated with pubertal and growth delay. If growth failure is evident despite adequate supplementation, formal assessment of pubertal status and growth hormone levels is recommended. Treatment with growth hormone is likely to benefit those with true growth hormone deficiency if provided with optimized biochemical control.
让患者了解疾病原因和性质,是患者赋权至关重要的任务。这些信息可以通过各种途径提供,如:
- 临床环境中的个人教育;
- 宣传资料;
- 网络资料以及患者论坛(补充表S6);
- 患者和家庭团体的支持活动。
患者或护理人员都应该知道在如何处理紧急情况。佩戴医疗识别手环(例如,Medic-Alert,http://www.medicalert.org.uk/)可能(对实施急救)有帮助。旅行时,患者应随身携带医生证明,其中列出了所需的药物,并且不得阻止患者携带在随身行李中携带足够的钾镁补充剂药物。《患病守则》在发生中途发病时有帮助(补充表7)。(还有一个重要事项是),疾病在不同年龄段的有不同的情况,应向年轻病人重新说明。(儿童、青少年到成人的)过渡期护理诊所(TCC)的医生应建立对患者的疾病、治疗方法,以及对日常生活影响的认知和意识。应鼓励患者及其家属联络当地或区域性的患者组织(补充表6)。
Education about the cause and nature of the disease is critical for patient empowerment. This information can be provided through a variety of media, including:
- personal education in a clinical setting;
- information leaflets;
- web-based information and patient-led forums (Supplementary Table S6);
- patient and family groups’ support events.
Patients, their caregivers or both need to know what to do in case of an emergency. A medical identity bracelet (e.g., Medic-Alert, http://www.medicalert.org.uk/) may be useful. If traveling, patients should carry a doctor’s letter with them that lists medications required, and they must not be prevented from carrying adequate supplements for their journey in hand luggage. “Sick day rules” are helpful in case of intercurrent illness (Supplementary Table S7). It is important to reexplain the disease at different stages of life to the young adult. Physicians at transition clinics should build up awareness and consciousness of the patient’s disease and treatment and the implications thereof for daily life. Patients and their families should be encouraged to contact local or regional patient organizations (Supplementary Table S6).
GS可能会影响(患者儿童的)学校的表现(例如:缺席、注意力不集中)。已有一些国家制定了具体的措施,来弥补这些儿童的学校教育限制。这些措施应根据当地实际和个体情况制定和实施。
GS can compromise school performance (e.g., absence, difficulty in concentration). Country-specific measures exist to compensate schooling limitations of these children. They should be used or developed according to the local practice, on an individual basis.
GS还可以影响工作表现。在大公司中,当地的职业健康医生或可帮助患者根据其具体健康状况找到解决方案。例如,如果(GS导致的)乏力使得工作时间达不到8小时,则调整方式可以是提供额外的休息时间、减少工作时间或在家工作的能力。需要轮班的工作,GS患者可能会感觉特别困难。患者可能因为担心失去工作,而害怕透露自己的病情。但是,应鼓励患者分享有关其疾病的信息,同时必须向雇主提供了解GS的教育资源。
GS can also compromise work performance. In larger companies, local occupational health physicians may aid patients in finding solutions for their specific health situations. For example, if fatigue makes working an 8-hour day impossible, accommodations might include extra rest periods, reduced hours, or the ability to work at home. Work shifts may be particularly difficult for GS patients. Patients may be afraid to disclose their condition because they fear losing their job. However, patients should be encouraged to share information about their disease, but not without providing the employer with educational resources about GS.
没有证据表明参加体育运动对GS有害。但应谨慎参与需要耐力的或剧烈运动,或比赛项目。特别是应该避免容量不足,补充盐或电解质对此有所帮助。有心脏病表现或QT延长病史的患者,建议进行心脏病学检查。
There is no evidence suggesting that participation in sports is deleterious in GS. Caution is recommended in cases of endurance or strenuous exercise or competition practice. Volume depletion in particular should be prevented, and additional salt or electrolytes or both may help. In cases of history of cardiac manifestations or prolonged QT, a cardiology workup is advised.
总结和观点 Conclusion and perspectives
GS于1966年首次被描述,其遗传学原因在30年后被阐明。尽管对根源性肾脏机制已经有了可靠的理解,但临床严重程度差异很大,就算是生化指标的异常程度相似, 有的患者基本上无症状只是偶然诊断发现,有的则严重残疾。这仍然是未解之谜。更好地理解这种多变性中所涉及的因素,对于提供更好的治疗方法至关重要。鉴于大量的偶然诊断,可以推测GS可能存在严重的漏诊。表4中列出了已确定的知识空缺,和研究议程建议。GS基本上与所有罕见疾病一样,支持循证治疗的(资源)始终是有限的。本次会议产出中提供的大多数指南,或是基于临床经验,或是观察性研究,或是病例报告。因此是从质量较差的证据中得出的结论。我们充分意识到,本次会议提供的指南将随着时间的推移进行修订。不过,这些建议代表了我们目前的知识水平,并建立了一个初始框架,以进行临床审计,从而实现质量控制,为未来的治疗提供比较和衡量的(参照)。
GS was first described in 1966, and its genetic basis was elucidated 30 years later. Despite a solid understanding of the underlying renal mechanism, the wide spectrum of clinical severity, ranging from incidental diagnosis in essentially asymptomatic patients to severe disability in others despite similar biochemical abnormalities, remains an enigma. A better understanding of the factors involved in this variability is critical to provide better treatments. Given the high numbers of incidental diagnoses, it is tempting to speculate that there may be significant underdiagnosis of GS. A list of identified knowledge gaps and proposals for a research agenda are provided in Table 4. As with essentially all rare diseases, support for evidence-based treatment in GS is limited at best. Most of the guidance provided in this conference output is based on clinical experience, observational studies or case reports and is therefore derived from low-grade evidence. We are fully aware that the guidance provided here will be revised with time. However, these recommendations represent our current state of knowledge and constitute an initial framework to enable clinical auditing and thus quality control for which future treatments can be compared and measured against.
表4 | Gitelman综合征的知识空缺和研究课题
Knowledge gaps and research questions for Gitelman syndrome
诊断和生物标志物
1. 尿液外泌体,包括NCC和pNCC的评估
1. 造成钾、钠、氯的丢失的尿液值或肌酐比(随机尿)
1. 镁离子与总镁测量的比值
Diagnostic and biomarkers
1. Urinary exosomes, including assessment of NCC and pNCC
1. Urine values or creatinine ratios establishing wasting for potassium, sodium, chloride (spot)
1. Value of ionized versus total magnesium measurement
|
| —- |
|
临床方面
1. 血压控制,高血压(发病率,病因等)
1. 心血管并发症:传导、心肌、基于心电图的(病情)预测,可重复性,年龄因素,QT间期和电解质水平
1. 代谢并发症:葡萄糖耐量,镁平衡的作用
Clinical aspects
1. Blood pressure control, hypertension (incidence, cause, etc.)
1. Cardiovascular complications: conduction, myocardium, predictive effort ECG, reproducibility, age effect, QT interval, and electrolyte levels
1. Metabolic complications: glucose tolerance, role of magnesium balance
|
|
与患者相关的结局
1. 生活质量,残疾,社会学,症状认知能力
1. 残疾评分
1. 自我管理技能
Patient-related outcomes
1. Quality of life, disability, sociology, perception of symptoms
1. Disability scores
1. Self-management techniques
|
|
遗传学方面
1. 遗传异质性,致病基因或修饰基因
1. 评估各种变异的致病性
1. 外显子组数据库中SLC12A3突变的患病率
1. 携带者状态的影响,地理差异的影响
1. 基因型 - 表型相关性,包括SLC12A3三重突变的影响
1. 性别影响
1. 确定发病率和携带率
Genetic aspects
1. Genetic heterogeneity, causal genes, or modifier genes
1. Assessment of the pathogenicity of variants
1. Prevalence of SLC12A3 mutations in exome database
1. Effect of the carrier state, geographic variations
1. Genotype-phenotype correlations, including effect of triple SLC12A3 mutations
1. Sex effect
1. Establishing prevalence of the disease and the carrier state
|
|
干预(治疗)
1. 高剂量NaCl补充的影响
1. 运动,增加肌肉量,运动后补钾的影响
1. 确定钾和镁的最佳目标值
Intervention
1. Effect of high NaCl supplementation
1. Effect of sport, increased muscular mass, potassium supplementation after exercise
1. Define optimal target values for potassium and magnesium
|
|
结局和自然病史
1. (病例)登记,(存入)生物银行
1. 成长,活动,体育运动
1. 葡萄糖不耐受,和代谢特征
1. 肾功能、尿浓缩功能缺陷、慢性肾病、囊肿
1. 心血管并发症
1. 罕见的并发症:假性脑瘤,漏斗胸,自身免疫相关疾病
Outcome and natural history
1. Registry, biobanking
1. Growth, activity, sports
1. Glucose intolerance and metabolic profile
1. Renal function, concentration defect, proteinuria, chronic kidney disease, cysts
1. Cardiovascular complications
1. Rare complications: pseudotumor cerebri, pectus excavatum, link with autoimmunity
|
|
母亲和儿童
Mother and child
Pregnancy and fetal development
|
|
监测
Monitoring
Improve monitoring: noninvasive, frequency, possible transcutaneous measurements
|
ECG,心电图;
NCC,噻嗪类敏感的钠氯协同转运蛋白;
pNCC,磷酸化的噻嗪类敏感的钠氯协同转运蛋白。
ECG, electrocardiogram;
NCC, thiazide-sensitive sodium-chloride cotransporter;
pNCC, phosphorylated thiazide-sensitive sodium-chloride cotransporter.
披露 Disclosure
DHE宣布已从辉瑞公司获得发言人酬金。NVAMK宣布获得了Seinen会议活动管理公司和Nutricia有限公司给与的发言人酬金,并获得了Eurenomics财团,荷兰卫生研究与发展组织和荷兰肾脏基金会的支持。MK宣布已收到Alexion制药和Otsuka制药的咨询费以及Alexion的发言人酬金。AB,D.Bockenhauer,D.Bolignano,LAC,EC,FEK,SHL,RVP和OD声明没有竞争性利益。
DHE declared having received speaker honoraria from Pfizer. NVAMK declared having received speaker honoraria from Seinen Congres Event Management and Nutricia GmBH and grant support from Eurenomics, Netherlands Organisation for Health Research and Development, and Dutch Kidney Foundation. MK declared having received consultancy fees from Alexion and Otsuka and speaker honoraria from Alexion. AB, D. Bockenhauer, D. Bolignano, LAC, EC, FEK, SHL, RVP, and OD declared no competing interests.
致谢 Acknowledgments
本报告献给并怀念Bartter和Gitelman综合征的主要临床研究者Alberto Bettinelli医生。
We dedicate this report to the memory of Dr. Alberto Bettinelli, a leading clinical researcher on Bartter and Gitelman syndromes.
补充材料 Supplementary Material
表1:转换表 Conversion table
表2:儿童尿钙/尿肌酐比的正常范围 Normal ranges of urinary calcium-creatinine ratio in children
表3:富含钾的食物,及其葡萄糖、镁、卡路里含量 Foods rich in potassium, with glucose, magnesium, and caloric content
表4:各种盐化合物的镁含量 Magnesium content by various salts
表5:富含镁的食物,及其葡萄糖、钾和卡路里含量 Foods rich in magnesium, with glucose, potassium, and caloric content
表6:Gitelman综合征患者的网络资源列表 List of web resources for patients with Gitelman syndrome
表7:《发病日守则》 Sick day rules
补充材料已链接到本论文的在线版本: www.kidney-international.org
补充表1:转换表
| 参数 | 国际标准单位 | 换算系数 | 公制单位 |
|---|---|---|---|
| 镁 | mmol/l | 2.43 | mg/dl |
| 钾 / 肌酐 | mmol/mmol | 8.84 | mmol/g |
| 钙 / 肌酐 | mmol/mmol | 0.3547 | mg/mg |
补充表2:儿童尿钙/尿肌酐比的正常范围
| 年龄 | 尿钙/尿肌酐(mmol/mmol) (5 - 95百分位) |
尿钙/尿肌酐 (mg/mg) (5 - 95百分位) |
|---|---|---|
| < 1 | 0.09-2.2 | 0.03-0.78 |
| 1 - 2 | 0.07-1.5 | 0.02-0.53 |
| 2 - 3 | 0.06-1.4 | 0.02-0.50 |
| 3 - 5 | 0.05-1.1 | 0.02-0.39 |
| 5 - 7 | 0.04-0.8 | 0.01-0.28 |
| 7 - 17 | 0.04-0.7 | 0.01-0.25 |
creatinine ratios in a healthy pediatric population. The Journal of Pediatrics, 131(2), 252–257.pdf
补充表3:富含钾的食物,及其葡萄糖、镁、卡路里含量
| 每获得1000mg钾需要的食物量 | 同时含有 | ||||
|---|---|---|---|---|---|
| 种类 | 重量(g) | 约为 | 卡路里(kcal) | 葡萄糖(g) | 镁(mg) |
| 炒黄豆 | 68 | 1/3 份 | 322 | 23 | 99 |
| 四季豆 | 270 | 1.5 份 | 349 | 65 | 151 |
| 小扁豆 | 271 | 1 份 | 314 | 54 | 98 |
| 鳕鱼 | 230 | 1 份 | 265 | 0 | 62 |
| 香蕉 | 280 | 2 个 | 249 | 64 | 54 |
| 赤豆 | 391 | 2 份 | 332 | 63 | 109 |
| 食用蜗牛 | 262 | 2 份 | 236 | 5 | 654 |
| 杏脯 | 86 | 2 份 | 207 | 54 | 28 |
| 草莓 | 654 | 3 份 | 216 | 50 | 85 |
| 花生 | 152 | 3 份 | 889 | 33 | 267 |
| 橙汁 | 543 | 1/2 升 | 255 | 60 | 54 |
| 无花果干 | 147 | 4 份 | 366 | 94 | 341 |
| 洋蓟 | 350 | 4 份 | 185 | 42 | 147 |
| 南瓜子 | 124 | 4 份 | 691 | 14 | 732 |
| 巧克力果馅饼 | 543 | 4 份 | 772 | 125 | 98 |
| 榛子 | 132 | 4 份 | 856 | 24 | 229 |
| Espresso意式咖啡 | 870 | 5 份 | 17 | 0 | 696 |
| 苹果汁 | 990 | 1 升 | 455 | 109 | 50 |
| 坚果谷物麦片 | 210 | 7 份a | 780 | 149 | 214 |
| 黑巧克力 | 120 | 1,2 板 | 604 | 36 | 394 |
| 谷物面包 | 435 | 2 条法棍 | 1152 | 187 | 339 |
| 椰子肉 | 281 | 3/4 个 | 994 | 42 | 90 |
| 椰子汁 | 400 | 2 1/2 杯 | 76 | 12 | 100 |
大约提供1000毫克钾元素所需的食物量,以及卡路里,葡萄糖和镁的含量。 并给出了相应的等同份量以便估计。例如,需要68g炒黄豆(约1/3份)以提供1g钾,并且还提供了322卡路里,23g葡萄糖和99mg镁。 数据来自网站http://aliments.monalimentation.org/ 计算出的镁和钾含量及等同份量。
a 每份30g包括牛奶
补充表4:各种盐化合物的镁含量
| 镁盐种类 | 分子量 | 镁元素% | 每克药物含镁量(mg) | 每克药物含镁量(mEq) | 获得50mEq需要的药物(g) | 生物利用度 |
|---|---|---|---|---|---|---|
| Gluconate葡萄糖酸镁 | 414.6 | 6% | 55 | 5 | 11 | 19% |
| Orotate 乳清酸镁 | 334.5 | 6% | 62 | 5 | 10 | |
| Malate 苹果酸镁 | 156.4 | 7% | 65 | 5 | 9 | |
| Aspartate 天冬氨酸镁 | 288.5 | 8% | 84 | 7 | 7 | |
| Glycinate 甘氨酸镁 | 172.4 | 9% | 90 | 7 | 7 | |
| Sulfate 硫酸镁 | 120.4 | 10% | 100 | 8 | 6 | 4% |
| Lactate 乳酸镁 | 202.5 | 12% | 120 | 10 | 5 | 41% |
| Chloride 氯化镁 | 95.2 | 12% | 120 | 10 | 5 | 20% |
| Glycerophosphate 甘油磷酸镁 |
194.4 | 13% | 125 | 10 | 5 | |
| Pidolate焦谷氨酸镁 | 280.5 | 16% | 160 | 13 | 4 | |
| Citrate 枸橼酸镁 | 214.4 | 16% | 160 | 13 | 4 | 16% |
| Hydroxide 氢氧化镁 | 58.3 | 42% | 420 | 34 | 1 | |
| Carbonate 碳酸镁 | 84.3 | 45% | 450 | 37 | 1 | 30% |
| Oxide 氧化镁 | 43.3 | 60% | 600 | 49 | 1 | 4% |
生物利用度数据来自Firoz M 和Graber M. Magnes Res 2001;14:257-262; Walker AF et al. Magnes Res 2003;16:183-191; https://www.gwh.nhs.uk/media/226663/oral-magnesium-preparations-for-the-treatment-and-prevention-of-hypomagnesaemia-ukmi-qas.pdf 等网站
数据已四舍五入
补充表5:富含镁的食物,及其葡萄糖、钾和卡路里含量
| 每获得100mg (4 mmol) 镁需要的食物量 | 同时含有 | ||||
|---|---|---|---|---|---|
| 种类 | 重量(g) | 约为 | 卡路里(kcal) | 葡萄糖(g) | 钾(mg) |
| 食用蜗牛 | 40 | 1/3 portion | 36 | 1 | 153 |
| 大豆 | 120 | 1/2 portion | 201 | 12 | 599 |
| 南瓜子 | 20 | 1/2 portion | 94 | 2 | 137 |
| Espresso意式咖啡 | 125 | 1 cup | 3 | 0 | 144 |
| 四季豆 | 180 | 1 portion | 230 | 43 | 661 |
| 鲭鱼 | 100 | 1 portion | 270 | 0 | 413 |
| 无花果干 | 40 | 1 portion | 107 | 28 | 293 |
| 小扁豆 | 280 | 1.5 portions | 322 | 56 | 1025 |
| 花生 | 60 | 1.5 portions | 332 | 13 | 374 |
| 赤豆 | 360 | 1.5 portions | 304 | 57 | 914 |
| 鳕鱼 | 370 | 2 portions | 426 | 0 | 1607 |
| 榛子 | 60 | 2 portions | 373 | 10 | 436 |
| 生菠菜 | 130 | 2 portions | 29 | 5 | 706 |
| 香蕉 | 370 | 2 1/2 medium | 330 | 85 | 1326 |
| 椰子汁 | 400 | 2 1/2 glasses | 76 | 12 | 1000 |
| 黑巧克力 | 30 | 3 squares | 153 | 9 | 254 |
| 谷物面包 | 130 | 3 small slices | 340 | 55 | 295 |
| 橙汁 | - | 1 liter | 470 | 110 | 1840 |
| 苹果汁 | - | 2 liters | 920 | 220 | 2020 |
大约提供100毫克镁元素所需的食物量,以及卡路里,葡萄糖和钾的含量。 并给出了相应的等同份量以便估计。例如,需要40g食用蜗牛(约1/3份)以提供100毫克镁,同时还提供了36卡路里,1g葡萄糖和153 mg钾。 数据来自网站http://aliments.monalimentation.org/ 计算出的镁和钾含量及等同份量。
补充表6:Gitelman综合征患者的网络资源列表
补充表7:《发病日守则》
|
除非医生建议,否则不要停药。
如因任何原因感到不适,请尽快检查你的钾、镁指标。
如果发生腹泻或呕吐,请增加液体摄入。但要确保在你喝的任何液体里,都加入少许盐,或电解质粉末。
如果持续呕吐,且超过24或以上无法进食,请立即就医。
此外,如失去知觉/昏倒,请立即就医。
或发生以下情况,且额外增加钾/镁补充剂用药后症状没有缓解的,请立即就医:
- 头晕目眩
- 感觉刺痛或肌肉无力
- 感觉心跳不规则(心悸)
- 痛感明显的肌肉痉挛
如果发现任何异样症状,请就医,可能您的药物剂量需要调整;一般简单的验血就可以。
|
| —- |

参考文献 References
https://www.kidney-international.org/article/S0085-2538(16)30602-0/fulltext#secsectitle006030602-0/fulltext#secsectitle0060)